Intra-Cytoplasmic Sperm Injection
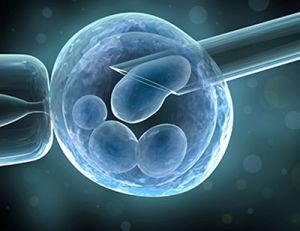
Intracytoplasmic sperm injection (ICSI) can be used as part of an in vitro fertilization (IVF) technique to help you conceive . ICSI is the most successful form of treatment for male infertility and is used in nearly half of all IVF treatments. ICSI takes one sperm, which is injected directly into the cytoplasm of the oocyte (egg). The fertilized egg (embryo) is then transferred to your uterus (womb). Male Infertility includes Aspermia - complete lack of semen Asthenozoospermia - reduced sperm mobility Azoospermia - absence of sperm cells in semen Hyperspermia - large semen volume Hypospermia - small semen volume Oligozoospermia - few spermatozoa in semen Necrozoospermia - dead or immobile sperms Teratozoospermia - sperm with abnormal morphology
...more
Best Ivf Centre In Mumbai

Y-Microdeletion Treatment
Y chromosome microdeletion (YCM) is a family of genetic disorders caused by missing gene(s) in the Y chromosome. Many men with YCM exhibit no symptoms and lead normal lives. However, YCM is also known to be present in a significant number of men with reducedfertility. Men with reduced sperm production (in up to 20% of men with reduced sperm count, some form of YCM has been detected) varies from oligozoospermia, significant lack of sperm, or azoospermia, complete lack of sperm.
...more
Uterine Fibroids Treatment
Fibroids are benigen tumours of the uterus made up of fibrous tissue. They arise in the myometrium, protrude in the uterine cavity or outside the uterus. Their size varies from 1 to 30 cm or even more. When fibroids are present in the myometrium pelvic pain, heavy uterine bleeding, dysmenorrhea and infertility are the chief symptoms. It is better to remove fibroids surgically ( myomectomy ) before starting fertility treatment. When fibroids are less than 5 cm and less than 3 in number can be removed by laproscopy. (lap-myomectomy) women with fibroids and infertility have a good chance of conception after myomectomy. Sometimes these myomas regrow and may need repeated surgery
...more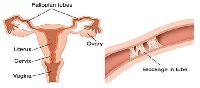
Tubal Blockage Treatment
Approximately 20% of female infertility can be attributed to tubal causes.[1] Distal tubal occlusion (affecting the end towards the ovary) is typically associated with hydrosalpinxformation and often caused by Chlamydia trachomatis.[1] Pelvic adhesions may be associated with such an infection. In less severe forms, the fimbriae may be aggluntinated and damaged, but some patency may still be preserved. Midsegment tubal obstruction can be due to tubal ligation procedures as that part of the tube is a common target of sterilization interventions. Proximal tubal occlusion can occur after infection such as a septic abortion. Also, some tubal sterilization procedures such as the Essure procedure target the part of the tube that is near the uterus.
...more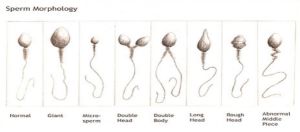
Teratospermia Treatment
Teratozoospermia, also known as teratospermia, is a semen alteration in which there is a large number of spermatozoa with abnormal morphology.It is a sperm condition that may lead to serious consequences, such as male infertility. The sperm parameter that is compromised is sperm morphology. The World Health Organisation (WHO) offers guidelines to evaluate semen parameters (some examples of these parameters are concentration, motility, or morphology). The values set by WHO can be used to determine normality, so if the value of a given semen parameter is below the reference, it may suggest a sperm pathology. With regard to teratozoospermia, the shape of the spermatozoon is assessed. Formerly, teratozoospermia was diagnosed if 14% of the sperm had a normal shape. In 2010, WHO updated its reference values, and now a man only has to meet a 5% rate of properly shaped spermatozoa to be within normality. Therefore, in order to diagnose teratozoospermia by the current standards, a man has to show a high rate of dysfunctional spermatozoa; more than 96% of his spermatozoa have to be morphologically abnormal.
...more
semen
MALE FACTOR : Semen– Human semen is 3-5 ml white liquid containg 40-100 million sperms. When sperms count is good the semen has a good viscocity. If there no sperms the semen is thin and watery. Soon after ejaculation the semen is viscous and in 5-10 mins it liquifes. When there is infection it is yellow in colour. Some men have ejaculatory dysfunction where the help of a sexual medicine doctor is taken. Common problem in semen are 1) low count – Oligospermia 2) Pus cells – Pyospermia 3) Low motility – Astheno Spermia 4) Dead sperms – Necro spermia 5) No sperms – Azoo spermia Normal sperm has > 40 million count , > 50% motile , ( grade 4 ) no pus cells , no becteria Sperms are produced in testis in highly colied tubes called Seminiferous Tubules. If we take a cut section of the seminiferous tubules we will find a layer of cells ( maturing spermatozoa ) in the cavity are seen sperms a sperm has head , neck , middle piece , tail. All seminiferous tubules open in a singal duct called Epididymus and sperms are carried through this tube in to another tube calle VAS DEFERENS to the male urethra. If there is a block any where in this route ( Epididymus to Vas Deferens ) even though the testis are producing sperms no sperms will be seen in the semen this is called OBSTRUCTIVE AZOOSPERMIA. In such men testicular size and consistency is normal but no sperm seen in semen. If we check the hormones : FSH + LH there serum levels are normal. These men can have baby with there sperms by using ICSI technique. Sperm are aspirated from the testis using a fine needle and used in ICSI technique.
...more
Premature Ovarian Failure Treatment
premature ovarian failure ( premature menopause. ) when the number of eggs in the ovary reduces dramatically, ovaries become small, and on 2nd day of menses the number of follicles in the ovary are less than 4. if we do amh levels (anti mullerian hormone) it is low < 1. all this normally happens when a women crosses 45 yrs of age – natural onset of menopause. in some women this process starts early and menstrual cycles become irregular, scanty, sexual drive drops, and she is infertile. all the medicines like dheas are tried to increase ovarian reserves but not all succeed. for women with low amh, high fsh, and poor antral follicle count – ivf should be started early to get the quickest chance of pregnancy.
...more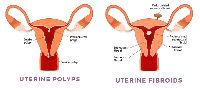
Polyps Treatment
Polyps: They are small cellular structures that grow in the inner wall of the uterus. Over growth of cells in the endometrium leads to uterine polyps. Small polyps don’t interfere in the reproductive process; whereas large polyps need to be removed. Large polyps increase the risk of miscarriage. They are oval or round in shape and they remained attached to the endometrial wall. Symptoms of uterine polyps include heavy bleeding, spotting or bleeding between menstrual periods, infertility and vaginal bleeding after menopause. Small polyps might regress at any stage. There is no non invasive treatment for polyps
...more
Polycystic Ovarian Disease Treatment
Do you have irregular menstrual cycles ? a. Yes b. No are you obese with hair on upper lip and chin abdomen calf muscles. A. Yes b. No has your gynecologist has informed you that you have pcod. A. Yes b. No polycystic ovarian disease [pcod] polycystic ovarian disease (pcod) is a condition where a women is usually (not always) obese with irregular menses and male like hair distribution on the body (upper lip, chin, abdomen, calf muscles, inner thighs). On sonography the ovary has many peripheral follicles and ovarian volume is increased. There are two hormones coming from the pituitary gland (based at the base of the brain) fsh and lh, normally they are in 1: 1 proportion, in pcod, lh is three times higher than fsh. Due to which a lot of follicles starts growing in the ovary, in the ovary there are two types of cells surrounding the egg- 1) theca cells outside 2) granulosa cells inside around the oocyte lh hormone acts on the theca cells which produce male hormone testosterone. Normally testosterone is converted to estrogen because of fsh acting on granulose cells. In pcod because lh is high theca cells are more testosterone produce by these cells cannot be converted to estrogen. This high circulating testosterone produces obesity, male like features and failure of ovulation. There is a genetic link between pcod and insulin resistance and many pcod women have altered gtt (glucose tolerance test) and high circulating insulin.
...more
Pelvic Inflammatory Disease Treatment
The female reproductive track consists of a vagina, cervix, uterus, two fallopian tubes and ovaries. Of these the fallopian tubes are most delicate and can get infected leading to their damage and infertility. Normally infections to reproductive tract are sexually transmitted and lead to damage and infertility. Nature protects our reproductive tract in many was - • the vagina has a very acidic ph, • the cervix has a thick plug which disallows bacteria to enter the reproductive tract. • the uterine lining sheds at every menstrual cycle and does not allow infection to persist inside the uterus. There are some infections which can reach the fallopian tubes in spite of all this protection. These are bacteria called. • chlamydia • mycloplasma • gonococci chlamydia are the commonest sexually transmitted organisms. The male reproductive tract harbous these organisms and are transmitted to the female. In the female, they remain symptom less till they reach the fallopian tubes when she experiences pelvic pain. Bacterial infections change the inner lining of the fallopian tubes, cause scarring, obstruction,oedema and distention of tubes (hydrosalpinx).
...more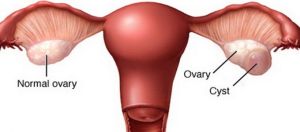
Ovarian Cyst Treatment
The ovaries are part of the female reproductive system. They’re located in the lower abdomen on both sides of the uterus. Women have two ovaries that produce eggs, as well as the hormones estrogen and progesterone. Most women will experience a cyst on the ovaries at least once, and most are painless, cause no symptoms, and are discovered during a routine pelvic exam. Symptoms of an ovarian cyst include nausea, vomiting, bloating, painful bowel movements, and pain during sex. In rare cases, an ovarian cyst can cause serious problems, so it’s best to have it checked by your doctor. There are various types of ovarian cysts, such as dermoid cysts and endometrioma cysts. However, functional cysts are the most common type. The two types of functional cysts include follicle and corpus luteum cysts.
...more
low sperm count treatment
Low sperm count means that the fluid (semen) you ejaculate during an orgasm contains fewer sperm than normal. A low sperm count is also called oligospermia. A complete absence of sperm is called azoospermia. Your sperm count is considered lower than normal if you have fewer than 15 million sperm per milliliter of semen. Having a low sperm count decreases the odds that one of your sperm will fertilize your partners egg, resulting in pregnancy. Nonetheless, many men who have a low sperm count are still able to father a child. The main sign of low sperm count is the inability to conceive a child. There might be no other obvious signs or symptoms. In some cases, an underlying problem such as an inherited chromosomal abnormality, a hormonal imbalance, dilated testicular veins or a condition that blocks the passage of sperm may cause signs and symptoms. Pretesticular azoospermia • Problems with sexual function — for example, low sex drive or difficulty maintaining an erection (erectile dysfunction) • Pain, swelling or a lump in the testicular area • Decreased facial or body hair or other signs of a chromosome or hormone abnormality.
...more
Klinefelter System Treatment
Klinefelter syndrome is a chromosomal condition that affects male physical and cognitive development. Its signs and symptoms vary among affected individuals. Affected individuals typically have small testes that do not produce as much testosterone as usual. Testosterone is the hormone that directs male sexual development before birth and during puberty. A shortage of testosterone can lead to delayed or incomplete puberty, breast enlargement (gynecomastia), reduced facial and body hair, and an inability to have biological children (infertility). Some affected individuals also have genital differences including undescended testes (cryptorchidism), the opening of the urethra on the underside of the penis (hypospadias), or an unusually small penis (micropenis).
...more
IVF Treatment In Mumbai
IVF Hospital In Mumbai defines In vitro Fertilization meaning fertilization outside the human body, IVF is a technique of assisted reproduction that is used for sub fertile couples. Consult an IVF Specialist in Mumbai today. In vitro Fertilization meaning fertilization outside the human body, IVF is a technique of assisted reproduction that is used for sub fertile couples. In IVF the oocyte and washed sperms are kept in a petri dish for fertilization. The fertilised ovum is then left in the culture medium to grow from day 2 to day 6. Depending on the case the embryos are transferred in the uterus to implant. Process of IVF takes about 20 days. It starts with controlled ovarian stimulation in which the ovaries are stimulated numerous follicles grow for about 10 days followed by an LH trigger. 35 to 36 hours after the LH trigger oocytes are retrieved. The sperm sample is prepared for IVF and the retrieved eggs are added in the semen sample and kept in the incubator for fertilization. The embryos are grown for 2 to 6 days and then transferred. IVF is usually advised to patients with infertility due to female factors. Patients who are advised donor egg or surrogacy will also go for IVF. Couples who will benefit from IVF • Tubal Blockage (single or both). • Borderline male sperm count. • Women with premature ovarian failure ( Donor egg IVF) • Advanced maternal age • Women with endometriosis • Unexplained infertility (Couple trying to conceive for more than 2 years but unable to conceive without any cause ) • Recurrent Pregnancy Loss
...more
Intrauterine Insemination
Intra uterine insemination (IUI) is leaving washed sperm sample inside the uterus , close to the fallopian tube. IUI is the basic treatment of infertility. It starts with ovulation induction followed by a LH trigger , post which semen sample is collected from the male partner , washed and insemimated in the wife’s uterus. The growth and the rupture of the follicles in monitored on ultrasound. Tubal patency is essential while doing IUI treatment , which are generally checked on X-ray or during a diagnostic laproscopy. Steps Involved During IUI 1.Ovulation Induction Starts from day 2 of the patients periods, she is given medication to grow more than one follicle. When the follicle size becomes 18 – 20 mm , a rupturing trigger is given to the female partner post which IUI is performed. 2.Semen Preparation The semen sample is washed in a media chosen depending on the semen count. The washed sample of then centrifuged to collect highest concentration of sperms in minimum amount of media, this is then loaded in a Catheter. 3.Insemination Some clinics do IUI once post or pre rupture, however at Jilla’s IVF we usually do IUI twice pre and post rupture follicular rupture and thus giving our patients a higher chances of conception.
...more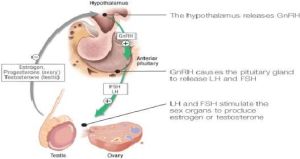
Hypogonadotropic Hypogonadism Treatment
Normally the ovarian follicle which consist of oocyte (eggs) granulose and theca cell, start producing estrogen (female sex hormone) in response to FSH & LH from pituitary. As the ovarian follicle grows, blood levels of estrogens rises, this estrogen supplies release of FSH and at a higher level causes LH surge and the follicle rupture, oocyte is released and what remains behind is crumpled granulosa and theca cells form the corpus luteum. Corpus luteum produces progesterone and its life is for 14 days. So 14 days often ovulation corpus luteum dies – progesterone levels fall – the inner lining of the uterus which was supported by progesterone sheds out as menstruation. So, for ovulation and menstruation to occur – pituitary FSH &LH are essential. When pituitary cannot produce FSH&LH – the condition is called Hypogonadotrophic Hypogonadism (HH). In this condition, women fail to get regular menses. Hypogonadotrophic Hypogonadism (HH) if mild, scanty menses occur at irregular intervals. Hypogonadotrophic Hypogonadism (HH) if severe, women will have no menses at all. Diagnosis is done by measuring serum FSH & LH levels which are usually less than 1 MIU/ML. Treatment of this condition is very rewarding. In women desiring fertility, ovulation is induced by injection of FSH & LH. Ovulation is monitored by Transvaginal ultra sound. Pregnancy rates are very high in these patients.
...more
Hyperprolactinemia Treatment
Prolactin is a hormone secreted from the PITUITARY gland to produce breast milk. When Prolactin levels are high, Pitutrary does not secrete FSH + LH hence ovulation does not occur. This happens normally during Lactation. In some women a small pituitary tumour secretes excessive Prolactin resulting in breast milk secretion, scanty menses or no menses and infertility. CABERGOLINE is drug of choice to treat these small adenomas. If the tumour is large (rarely) surgery is required.
...more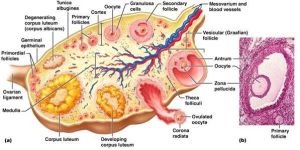
Follicular Study
A womens ovary has 6 million oocytes at puberty. At every menstrual cycle a group of antral follicles, 10-15 in number start growing. An antral follicle consists of an oocyte (female egg) surrounded by granulosa and theca cells (two types of cells)- which nourishes the oocyte and secrete female hormone called estrogen. As estrogen collects around the oocyte the antral follicles look like small fluid filled cysts. They grow at a rate of 2 mm per day, by the 5th or 6th day of menstrual cycle, majority of these antral follicles undergo artesia and only one grows. This growing follicle can be seen by Transvaginal ultrasound daily- This is called follicular study. The study starts around 8th to 10th day of menstrual cycle and continues till the follicle ruptures. It usually ruptures after it achieves 20 mm size. In regularly menstruating women, follicle ruptures 14 days before expected menses; that is follicle will rupture on 16th day in a women who has 30 days cycle. With rupture of the follicle, oocyte with few granulosa cells falls out of the ovary and is picked up by the fallopian tube.
...more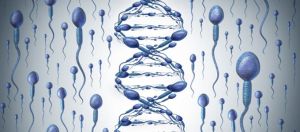
DNA Fragmentation Index
Sperm DNA fragmentation The genetic integrity of the spermatozoan is essential for normal embryo development. A high level of DNA fragmentation in sperm cells may represent a cause of male infertility that conventional examinations - sperm concentration, motility analysis, morphology assessment - cannot detect. Results reported in the scientific literature show regardless of the assisted reproductive technology used, elevated levels of DNA fragmentation above the critical threshold will significantly compromise the possibility of a successful pregnancy. High sperm DNA fragmentation does not appear to affect fertilisation or the first or second embryo cleavage stages High sperm DNA fragmentation can affect embryo cleavage once the paternal genome is switched on, and subsequent blastocyst development DNA fragmentation levels are closely correlated with IUI, IVF and ICSI miscarriage and pregnancy rates DNA fragmentation is significantly higher in sub fertile men. Men with poor semen parameters are more likely to have high DNA fragmentation High sperm DNA fragmentation is also found in men with normal semen parameter
...more
Azoospermia Treatment
Azoospermia may occur because of reproductive tract obstruction (obstructive azoospermia) or inadequate production of spermatozoa, such that spermatozoa do not appear in the ejaculate (non-obstructive azoospermia). Azoospermia is diagnosed based on the absence of spermatozoa after centrifugation of complete semen specimens using microscopic analysis. Azoospermia can be classified into three major types as listed. Many conditions listed may also cause various degrees of oligospermia rather than azoospermia. Pretesticular azoospermia Pretesticular azoospermia is characterized by inadequate stimulation of otherwise normal testicles and genital tract. Typically, follicle-stimulating hormone (FSH) levels are low (Hypogonadotrophic) commensurate with inadequate stimulation of the testes to produce sperm. Examples include hypopituitarism (for various causes), hyperprolactinemia, and exogenous FSH suppression by testosterone. Chemotherapy may suppress spermatogenesis. Pretesticular azoospermia is seen in about 2% of azoospermia Testicular azoospermia In this situation the testes are abnormal, atrophic, or absent, and sperm production severely disturbed to absent. FSH levels tend to be elevated (hypergonadotropic) as the feedback loop is interrupted (lack of feedback inhibition on FSH). The condition is seen in 49-93% of men with azoospermia. Testicular failure includes absence of failure production as well as low production and maturation arrest during the process of spermatogenesis.
...more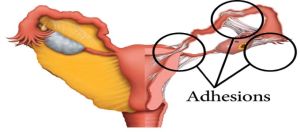
Ashermans Syndrome Treatment
Intrauterine adhesions, or intrauterine synechiae, are a condition in which scar tissue develops within the uterine cavity. Intrauterine adhesions accompanied by symptoms (e.g. infertility, amenorrhea) are also referred to as Asherman syndrome. The degree of adhesion formation and the impact of the adhesions on the contour of uterine cavity vary greatly. With minimal disease, thin bands of tissue stretch between surfaces of the uterine cavity, whereas severe disease is characterized by complete obliteration of the cavity, with the anterior wall of the uterus densely adherent to the posterior wall. These may impede menstrual flow or interfere with conception or pregnancy.
...more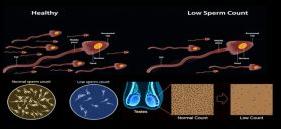
Abnormal Sperm Infertility
Low sperm count means that the fluid (semen) you ejaculate during an orgasm contains fewer sperm than normal. A low sperm count is also called oligospermia. A complete absence of sperm is called azoospermia. Your sperm count is considered lower than normal if you have fewer than 15 million sperm per milliliter of semen. Having a low sperm count decreases the odds that one of your sperm will fertilize your partners egg, resulting in pregnancy. Nonetheless, many men who have a low sperm count are still able to father a child. The main sign of low sperm count is the inability to conceive a child. There might be no other obvious signs or symptoms. In some cases, an underlying problem such as an inherited chromosomal abnormality, a hormonal imbalance, dilated testicular veins or a condition that blocks the passage of sperm may cause signs and symptoms. Pretesticular azoospermia • Problems with sexual function — for example, low sex drive or difficulty maintaining an erection (erectile dysfunction) • Pain, swelling or a lump in the testicular area • Decreased facial or body hair or other signs of a chromosome or hormone abnormality.
...more
ivf center

Infertility Treatment

Laser Assisted Hatching Treatment
Laser assisted hatching Laser assisted hatching is a technique done in the laboratory with the use of laser, where the zona is drilled and a gap is made in the zona (zona is the shell of the embryo). This is done before embryo transfer, the idea is that a small part of the trophectoderm starts protruding out so as to help the embryo attach to the endometrial tissue Hatching can be done in 3 ways : 1. With acid tyrode’s solution 2. Mechanically dissecting a small portion of the zona 3. Using laser Some studies show that laser assisted hatching does improve the success rate of IVF by improving the implantation rate. Some studies also say that laser assisted hatching also improves the implantation rate of frozen embryos
...moreBe first to Rate
Rate ThisOpening Hours